2 min read
Evaluation and Management (E/M) Coding Based on Time
Hope Bonnetti : Aug 28, 2023 5:43:11 PM

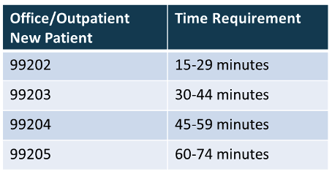
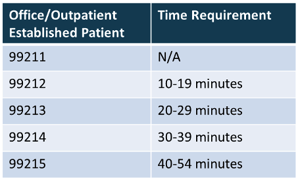
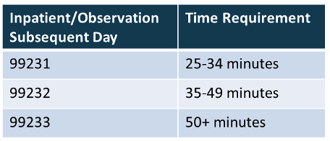
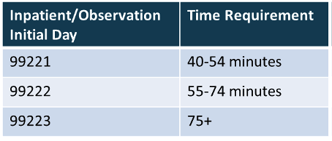
In 2021 and 2023, time-based E/M service guidelines underwent significant revisions for office/outpatient and inpatient/observation services. The Centers for Medicare and Medicaid Services (CMS) and the American Medical Association (AMA) CPT® guidelines came to a ground-breaking agreement to streamline and simplify E/M service guidelines, especially those based on time.
Overview
Time has continued to be a valid method for determining an E/M service level. However, everything else has changed. Time is defined as the total time a physician or other qualified health care professional spends rendering services/caring for a patient on a given calendar date. Providers may count all time, including, face-to-face, non-face-to-face, unit/floor, or off unit/floor time towards their overall level of service, if that time occurs on the same calendar date as the patient visit. Qualifying time activities, include, but are not limited to:
- Preparing to see the patient (review of previous test results, history)
- Obtaining and/or reviewing separately obtained history
- Performing a medically appropriate exam and/or evaluation
- Care coordination
- Counseling and educating the patient, family, or caregiver
- Independently interpreting results (not separately reported) and communicating results to the patient, family, or caregiver
- Ordering medications, tests, or procedures
In addition, time-based services are no longer required to be dominated, greater than 50%, by counseling and/or coordination of care. This is a huge win for providers, as it now allows reimbursement for work that previously went unpaid based solely on the location of where the provider performed that work (“pajama time” at home). The elimination of counseling and/or coordination of care requirements is also beneficial, reducing the additional cognitive burden of tracking the percentage of time spent performing those activities.
Documentation Tips
Another improvement for time-based services is the simplification of documentation requirements. Per CMS, at a minimum, if a provider is leveling based on time, all they need to identify within their documentation is total encounter time, of course in addition to the details of their medically appropriate evaluation. Time should be as near exact as possible, no rounding-up of time is permissible.
Although not a requirement, it may be best practice to identify the activities in which the time was spent, such as, “Total time spent on today’s encounter, 30 minutes, included a face-to-face evaluation, record review, and documenting.” Furthermore, if separately reported procedures are also performed on the same date, you may want to consider adding an additional statement to your time-based phrase identifying the procedure time was carved out and/or excluded from your total time.
Keeping it simple, yet detailed, not only helps support why the time spent was required on external audit, but in today’s EMR world, patients have access to their notes almost instantaneously. If a patient spends 15 minutes with you but sees you have documented and billed for a 45-minute visit, that could cause additional headaches not only for you, but your front office and billing staff, as well.
Use It, Don’t Abuse It!
Be mindful that you don’t misuse or overuse time-based leveling. On paper it seems great, and so much easier to follow than the complex world of medical decision making (MDM) guidelines. However, it may not be beneficial as highly complex patients can be managed in less time than would be required.
Many EMRs offer leveling tools, including a time calculator to assist in capturing all activities spent on a date of service. While these tools can be helpful, they are by no means 100% accurate. EMR calculators track time spent having the patient’s chart open, but simply because the chart is open doesn’t mean you’re actively working on patient. The flip side is also a valid concern, the chart could be closed, so the calculator is not registering the time, yet you are on a phone call with another provider discussing patient management.
If you are mindful of your time spent rendering patient care on the date of service, select the appropriate E/M level based off that time, and document it appropriately, you will be compliant and accurately coding!